




Search | Sitemap | Navigation |  |
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
| ICHD-II 1.6 |
1.5.3 Persistent aura without infarction
Description:
Aura symptoms persisting for more than 1 week without radiographic evidence of infarction.
Diagnostic criteria:
A. The present attack in a patient with 1.2 Migraine with aura is typical of previous attacks except that one or more aura symptoms persists for > 1 week
B. Not attributed to another disorder
Comments:
Persisting aura symptoms are rare but well documented. They are often bilateral and may last for months or years. Reliably effective treatment is not known though acetazolamide and valproic acid have helped in a few cases. Exclude posterior leukoencephalopathy by diffusion MRI among other things. Exclude 1.5.4 Migrainous infarction by MRI.
Compendium taken from Cephalagia © International Headache Society 2003.
Persistent migraine aura without infarction - a detailed description
By Klaus Podoll, Markus Dahlem and David C. Haas (retired)
History of concept and terminology
Migraine aura status was not included among the sub-types of migraine listed in the 1988 classification of migraine by the International Headache Society (IHS), probably because the committee members were unaware of this condition. They did, however, list a class called migraine with prolonged aura. To be placed into this class, at least one of the patient's aura symptoms must last more than 60 minutes and less than 7 days.
In his 1982 report of two patients, David C. Haas used the term prolonged migraine aura status. Subsequent articles have used the following terms: 1. Sustained visual aura, 2. Persistent positive visual phenomena, 3. Persistent migraine aura, 4. Migraine aura status, 5. Persistent migrainous visual phenomena.
Finally, the Second Edition of the International Headache Classification by the IHS published in 2003 introduced the term 6. Persistent migraine aura without infarction for the aura status.
What are the symptoms?
The symptoms are those of a migrainous visual aura that either recurs repetitively hour-after-hour, day-after-day for weeks, months, or years, or does not abate for weeks, months, or years. Aura symptoms other than visual may be a part of the picture, but so far no one has reported a migraine aura status composed soley of non-visual aura symptoms.
Examples (abbreviated) from the medical literature
Repetitive variety
Patient 1 of Haas (1982): This 70-year-old man had stereotyped repetitive attacks several times per hour for about 5 weeks. His description of them is enhanced by his painted rendition of their appearance.
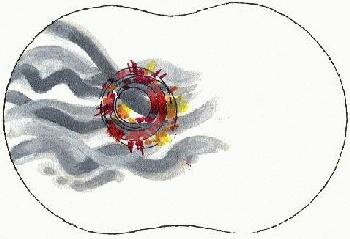
Illustration of visual patterns seen in prolonged migraine aura status by patient 1 of Haas (1982).
Each repetition began with slowly undulating thick gray lines, which changed in a few minutes into a pinwheel of bright whirling color in his left visual field. Several minutes later this image slowed down and disappeared. After more than a week of suffering these hallucinations, he also developed brief attacks of "electrical" paresthesias in his left hand. These were less frequent than the visual phenomena and alternated with them irregularly. Throughout his ordeal, he had a dull headache over his right eye.
The 7 patients with "aura status" reported by Haan et al.. (2000) experienced several mostly visual auras daily for weeks, very often without headache. They were asymptomatic between the auras.
Continuous variety
Case of Luda et al. (1991): This 65-year-old woman developed "scintillating scotomas" in her right visual field without headache on May 3, 1990 and they were still present and unremitting when the authors reported her problem over 12 months later. The hallucination was described as "scintillating geometrical figures (in the shape of either rings or chains)..."
Patient 3 of Liu et al. (1995): On November 10, 1992, this 29-year-old woman "experienced sudden disorientation followed by stars filling the visual field of both eyes, followed by a diffuse, nonpulsating headache. When the headache ceased, she was left with "constant flashing lights and circles which were worse at night..." These visual symptoms resolved spontaneously in April 1993. Months later, she experienced "zig-zag" lines for 10 minutes followed by a pulsating headache. She also had brief attacks of unilateral paresthesias sometimes followed by headaches both before and after the persistent aura.
Patient 1 of Chen et al. (2001): This 45-year-old woman reported seeing an occasionally flickering coin-sized white spot in her left field of view for 3 months. It began "after" a migraine headache without aura. It prevented reading.
Patient 2 of Chen et al. (2001):This 24-year-old woman complained of seeing numerous stars persistently flickering in her right visual field for 3 years. At times they formed a single light. This phenomenon developed during a migraine attack. She had suffered migraines from childhood. A visual aura of of bright yellow flickering stars lasting 30-60 seconds had occurred during most of her migraine headaches.
Patient of Spierings (2002): This 41-year-old man with migraine with typical visual aura from childhood developed his typical aura while upset in October 1996. It was unusually vivid and was accompanied this time by tingling in his left upper limb for 30 minutes. This was followed by severe headache with photophobia, generalized weakness, and confusion. The visual disturbance never disappeared, but has persisted to the time of Spiering's report. The patient sees things as though looking through a veil, and "bright-white, flickering, zigzag lines in the periphery of both visual fields" (his typical aura) come and go.
Continuous, strongly fluctuating variety
Patient 1 of Rothrock (1997): Two months before she was seen by the author, this 61-year-old woman experienced a particularly severe prolonged migraine with "jagged zigzags like crushed broken glass" to the left of a scotoma in her left visual field. This hallucination persisted after the headache ceased. It had been fluctuating in size, without disappearing entirely. In addition, she had developed similarly fluctuating but persistent numbness and tingling in the left face and lips.
Who gets these phenomena?
They can occur from childhood to old age. All reported patients had previously experienced either migraine headaches with visual auras, migraine visual auras without headache, or migraine headaches without auras, or various combinations of these migraine varieties.
What have brain tests−MRIs, EEGs, and SPECT scans−told us?
CT and MRI have not shown notable abnormalities. Thus, cerebral infarctions and tumors are well-excluded causes. EEGs on 21 patients showed abnormalities in only two, a father and daughter with occipital slow waves. So, the EEG evidence excludes an epileptic cause. SPECT scans have shown decreased cerebral perfusion in most of the patients scanned, and in those with phenomena in just one hemifield the decreases have been on the side opposite the perceptions (e.g. left field phenomena, right cerebral perfusion decrease). In some scans the perfusion decreases have been limited to the occipital lobe. These findings suggest that the affected cerebral regions are metabolically depressed, and they are compatible with the data from more quantitative tests in patients with typical migrainous auras.
Treatment
Patient number 1 reported by Haas in 1982 (see above) had his frequent repetitive visual attacks fade away quickly 2 days after he began taking cyproheptadine and after he failed to improve on acetylsalicylic acid. Three of the 7 patients of Haan et al. (2000) (see above) with repetitive attacks similar to those of Haas were treated with acetazolamide (250 mg twice or thrice daily) and all 3 experienced cessation of their auras in a matter of days. When the drug was discontinued or its dosage was lowered, the auras returned. None of their 7 patients responded to valproate or propranolol.
Rothrock (1997) reported the disappearance of persistent auras during treatment with divalproex in 2 patients, and Chen et al. (2001) reported the disappearance of persistent auras during treatment with lamotrigine in 2 patients. A host of other drugs have been unsuccessful, including phenytoin, phenobarbital, carbamezepine, acetylsalicylic acid, inbuprofen, verapamil, nifedipine, nimodipine, flunarazine, amitriptyline, clonazepam, fluoxetine, sertraline, baclofen, and buspirone. However, topiramate (Topamax) may be effective for some patients,as indicated in the following e-mail message received by David C. Haas on June 14, 2002:
"I've suffered from Migraine Aura Status (although I didn't know to call it other than just Migraine) for approximately 2 1/2 years. I've been treated quite successfully for this with Topamax. I began taking 50 mg twice a day in January 2001 and within a couple of weeks the visual phenomenon cleared up. This spring we decreased the dosage to 25 mg in the morning & kept the night dosage at 50 mg and within a week the visual symptoms began to return. I also experienced a migraine headache during this time. Needless to say, I'm back to the original dose and the symptoms have subsided."
Two continuous, prolonged migrainous visual auras, of 11 and 5 days duration were reported by Rozen (2000) to disappear within a few hours after an intravenous dose of 20 mg of furosemide. This drug was chosen, because it has been shown to inhibit the generation and duration of cortical spreading depression (the putative physiological cause of migrainous auras) induced by potassium in the cat. Although these two patients did not have migraine aura status as discussed above, perhaps they would have if left untreated.
The evidence so far suggests that acetazolamide may be the premier drug for patients with the repetitive form of aura status, and that divalproex (valproate), lamotrigine, or topiramate should be first choices for patients with the continuous form. When these oral drugs are ineffective, an intravenous injection or injections of furosemide should be tried.
Comment
David C. Haas has grouped both the repetitive and continuous forms of the prolonged visual migrainous auras under the rubric of migraine aura status since they both share the characterizing feature of affecting persons for weeks, months, or longer. Since the word "status" as used in "status epilepticus" means a prolonged condition, whether the seizures are repetitive or unremitting, its use for both of the prolonged aura states seems appropriate. Further studies might tell us whether these two aura states are basically the same condition or not.
Most of the materials of this webpage have originally been presented on the Upstate Medical University website Headache Cybertext: for the diagnosis and treatment of headaches and migraines by David C. Haas, removed from the web after his retirement December 31, 2004 (http://www.upstate.edu/neurology/haas/hpmiau_stat.htm, December 31, 2004).
References
Chen WT, Fuh JL, Lu SR, Wang SJ. Persistent migrainous visual phenomena might be responsive to lamotrigine. Headache 2001; 41: 823-825.
Evans RW, Lay CL. A persistent migraine aura. Headache 2000; 40: 696-698.
Haan J, Sluis P, Sluis LH, Ferrari MD. Acetazolamide treatment for migraine aura status. Neurology 2000; 55: 1588-1589.
Haas DC. Prolonged migraine aura status. Ann Neurol 1982; 11: 197-199.
International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988; 8 (suppl 7): 1-96.
International Headache Society. The International Classification of Headache Disorders, 2nd edition. Cephalalgia 2004; 24 (suppl. 1): 1-160.
Liu GT, Schatz NJ, Galetta SL, Volpe NJ, Skobieranda F, Kosmorsky GS. Persistent positive visual phenomena in migraine. Neurology 1995; 45: 664-668.
Luda E, Bo E, Sicuro L, Comitangelo R, Campana M. Sustained visual aura: a totally new variation of migraine. Headache 1991; 31: 582-583.
Rothrock JF. Successful treatment of persistent migraine aura with divalproex sodium. Neurology 1997; 48: 261-262.
Rozen TD. Treatment of a prolonged migrainous aura with intravenous furosemide. Neurology 2000; 55: 732-733.
Spierings EL. Flurries of migraine (with) aura and migraine aura status. Headache 2002; 42: 326-327.
Author: Klaus Podoll, Markus Dahlem and David C. Haas (retired)
Last modification of this page: Saturday March 12. 2005
| ICHD-II 1.6 |
 Top of the page
Top of the page| · | News |
| · | Medical Professionals |
| · | Medical Studies |
| · | Persistent migraine aura symptoms (visual snow) |
| · | Afterimages: See13 |
Copyright © 2005 Migraine Aura Foundation, All rights reserved. Last modification of this site: August 25, 2006
Thanks to: RAFFELT MEDIENDESIGN and GNU software | webmaster@migraine-aura.org
http://migraine-aura.org/EN/ICHD-II_1.5.3_Persistent_ma_wo_infarction.html


