




Search | Sitemap | Navigation |  |
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
Classification of visual disturbances
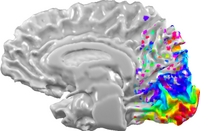
Visual cortex occupies large areas. The layout of the eccentric dimension of the retinal image is shown color-coded. © 2005 Jochem Rieger
Classification by prevalence of visual symptoms
Visual symptoms are by far most frequent in migraine with aura. From those who suffer from the aura almost everyone has experienced visual symptoms. Those with several types of aura symptoms have visual aura in the majority of their attacks, while the other modalities, like sensory, motor or aphasic symptoms are present only in a small fraction of their attacks (Russell and Olesen, 1996). This does not necessarily imply, however, that visual cortex is more susceptible for the aura, because a large cortical area is involved in visual processing (Tootell et al., 1996).
About 3% of the total volume of the human cortex is occupied by the primary visual cortex, also called striate cortex, or V1. An even much larger region is non-primary visual cortex (Sereno and Tootell, 2005). This "extra" non-primary cortex consists of multiple areas, denoted V2, V2, V3, V4, MST, MT, and by other abbreviations. Each area fulfills a rather specific functional task. It remains to be seen, whether the percentage area of cortex occupied by a specific sensory system matches the prevalence of the corresponding aura symptom.
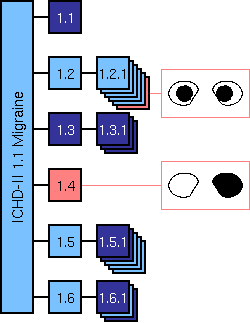
Migraine subtypes and subforms in which visual symptoms may appear (light blue). Only two migraine types (red) differentiate between the various visual symptoms.
Classification and diagnostic criteria of visual symptoms
Migraine is predominantly symptom-based divided into subtypes and further subdivided into subforms. Although visual disturbances are typical symptoms in two thirds of the migraine types ond forms, the set of diagnostic criteria that must be fulfilled does not differentiate between the various visual symptoms, except for retinal migraine and basilar-type migraine.
The ICHD-II classification for Migraine with aura is intended equally for clinical practice and research (Eriksen et al., 2005) and both, practice and research will help to improve it further. An important question is whether we can establish new diagnostic criteria for visual disturbances during migraine and use these as a basis for a new classification which can be matched against the ICHD-II. The objectives are twofold: characterize all phenotypes of visual symptoms, and establish the underlying neural circuitry. This may provide a first step towards an aetiological classification.
| cortical area | |||||
|---|---|---|---|---|---|
| V1 | V2 | V3 | V4 | ... | |
| CSD |  |
||||
| TIA | |||||
Table of a possible aetiological classification of aura symptoms.
Classification and aetiological factors
Different aetiologies, such as a transient ischemic attack (TIA) or cortical spreading depression (CSD) (see here) do not necessarily lead to completely different visual symptoms. That is because the hallucinatory percept is governed by neural correlates of conscious vision. These correlates and not the aetiology determine the percept, because different aetiological factors can lead to the same dysfunction of the neural circuits of these correlates.
For example, on a coarse spatial scale it is rather obvious that the site of the cortical origin determines the modality of a positive neurological symptom, i.e., whether something is seen, felt or heard etc, and likewise for negative neurological symptoms, i.e. whether a sensory input is not seen, not felt, or not heard.
Even on a finer spatial scale, i.e., within one modality−say the visual−the layout of the functional cortical maps determine the positive neurological symptoms. This is implied by Heinrich Klüver's notion of hallucinatory form constants (see here).
The functional maps are topographic maps of the sensory input, e.g. the topographic layout of the retinal image (retinotopy) or body surface (homunculus). An endogenous excitation within these maps can lead to a characteristic hallucinatory percept independent on aetiological factors that cause this excitation. Therefore, a neural network model of visual migraine aura can predict the typical zigzag pattern from endogenous activity in so-called cortical orientation maps with very little assumptions about the aetiological factors (Dahlem et al. 2000, see also here).
Despite of the statement above, aetiological factors are not at all hidden in the visual aura. For example, the spatial extend of the endogenous excitation in the cortex and its the growth rate usually depends on aetiology. In other words, a TIA or a CSD have different spatio-temporal excitation pattern within the cortical surface. Therefore, the spatio-temporal development of the aura symptoms, that is, the temporal order or spatial arrangement of positive and negative symptoms depend on aetiology (Dahlem and Müller, 2003, see also here). The spatio-temporal pattern is not specific for visual symptoms or any other modality but a clear signature of the unterlying aetiology. A new classification of visual disturbances should be based on this signature rather than on precepts that do not necessarily depend on aetiological factors.
Validation of a classification of visual disturbances
On the neural level, brain functions are best understood in the visual areas of the cortex. Therefore visual symptoms are likely to be involved in the search and validation for aetiological factors identifiable from morphology of migraine aura.

Retinotopy and functional subdivision of human cortical areas © 2005 Jochem Rieger
As argued above, the morphology of visual migraine aura provides hints of the cortical origin. The functional subdivision of human cortical areas and the layout of the retinal image (retinotopy) allow only certain aura shapes. A well known visual migraine aura, the so-called fortification spectrum, is likely to be caused in the primary visual cortex (V1) because only this area is not split along the horizontal meridian, and also because the cortical magnification factors predict well its spatio-temporal course (Grüsser, 1995 and Hassenstein).
Aura symptoms caused in higher non-primary visual areas will be more complex, e.g. if a cortical area that shows higher responses for intact than for scrambled images of objects is disturbed during migraine, a mosaic-like vision may be the result.

(left, top) A picture of a natural scene and its scrambled version (bottom), (right, top) ventral (middle) medial (bottom) lateral view of a cortical area that shows higher responses for intact than for scrambled images © 2005 Jochem Rieger
To achieve a characterization of all phenotypes, people suffering from transient visual disturbances must provide an objective measure. To date nearly all descriptions are retrospective and there are no guidelines to standardize diagnosis. Computer-assisted diagnostic procedures may in the future establish such diagnostic criteria. Preliminary results indicate that neural network models for simulating visual migraine aura have become sophisticated enough to constrain and validate possible underlying cortical circuitry (see section Pathomechanisms).
References
Dahlem MA, Engelmann R, Löwel S, Müller SC. Does the migraine aura reflect cortical organization? Eur J Neurosci 2000; 12: 767-770.
Dahlem MA, Müller SC. Migraine aura dynamics after reverse retinotopic mapping of weak excitation waves in the primary visual cortex. Biol Cybern 2003; 88: 419-424.
Eriksen MK, Thomsen LL, Olesen J. Sensitivity and specificity of the new international diagnostic criteria for migraine with aura. J Neurol Neurosurg Psychiatry 2005;76: 212-217.
Grusser OJ. Migraine phosphenes and the retino-cortical magnification factor. Vision Res 1995; 35: 1125-1134.
Russell MB, Olesen J. A nosographic analysis of the migraine aura in a general population. Brain 1996; 119: 355-361.
Sereno MI, Tootell RBH. From monkeys to humans: what do we now know about brain homologies? Current Opinion in Neurobiology 2005; 15: 135-144.
Tootell RB, Dale AM, Sereno MI, Malach R. New images from human visual cortex. Trends Neurosci 1996; 19: 481-489.
Author: Markus Dahlem
Last modification of this page: May 06, 2006
 Top of the page
Top of the page| · | News |
| · | Medical Professionals |
| · | Medical Studies |
| · | Visual Symptoms |
| · | Retinal Migraine |
| · | Basilar-type migraine |
| · | Morphogenesis |
| · | Computer Assisted Aura Acquisition |
Copyright © 2005 Migraine Aura Foundation, All rights reserved. Last modification of this site: August 25, 2006
Thanks to: RAFFELT MEDIENDESIGN and GNU software | webmaster@migraine-aura.org
http://migraine-aura.org/EN/Classification_of_visual_disturbances.html


